The Unending Bite: A Timeline of Humanity’s Battle With Malaria
The First Encounters – Ancient Times (Prehistory–500 CE)
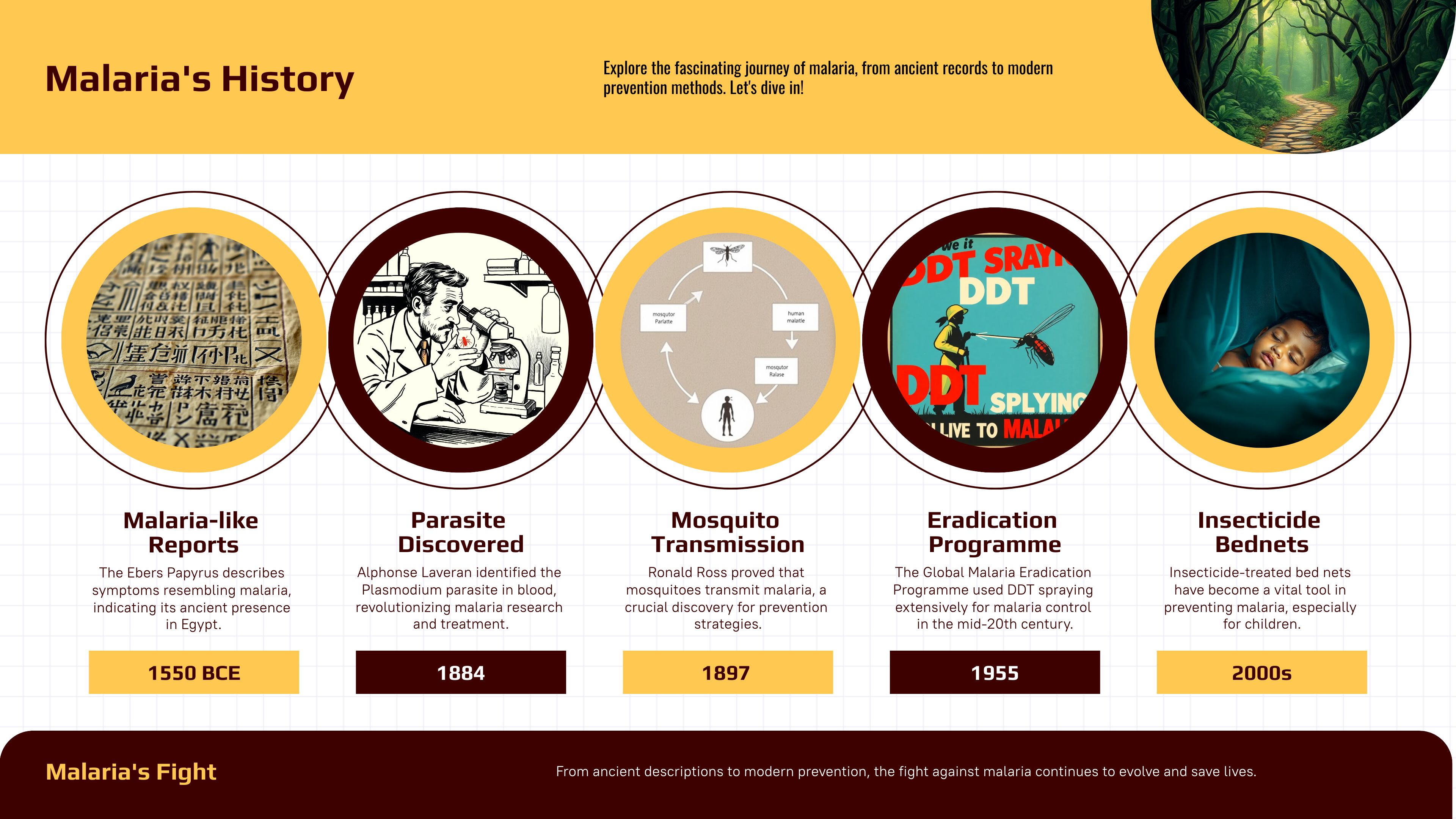
Evidence suggests malaria has plagued humans for millennia. While pinpointing the exact origin is difficult, genetic studies suggest that Plasmodium may have coexisted with humans since before the emergence of the human lineage, indicating a deep evolutionary relationship that predates Homo sapiens. The earliest written references to malaria-like illnesses appear in ancient Chinese texts from 2700 BCE. Descriptions of periodic fevers, chills, and splenomegaly, characteristic of malaria, also surface in Mesopotamian clay tablets (2000 BCE), Egyptian papyri like the Ebers Papyrus (circa 1550 BCE), and ancient Hindu texts (6th century BCE) (Carter and Mendis, 2002). These cultures often attributed the disease to supernatural forces or imbalances in the body’s humors, like “evil eye”, “black plague”, “evil wind”, or “evil humours”. The Greeks, notably Hippocrates and Galen, termed it “marsh fever,” noting its association with swampy environments and attributing it to “miasmata”—bad air (Carter and Mendis, 2002; Cox, 2010; Hempelmann and Krafts, 2013).
The Dawn of Scientific Inquiry (1600–1880)
While the miasma theory remained dominant, the burgeoning scientific revolution in Europe began to challenge established dogma. Antonie van Leeuwenhoek’s invention of the microscope in 1676 opened up a new world of microscopic observation, enabling the examination of blood and other bodily fluids. Though he likely observed microfilariae, not parasitic protozoa specifically related to malaria, his work laid the foundation for microscopy’s crucial role in future discoveries.
Quinine, derived from the bark of the cinchona tree, became an established malaria treatment in Europe during the 17th century. Its efficacy, though not understood at the time, provided the first effective treatment against the disease. Crucially, the connection between malaria and mosquitoes remained elusive. The prevailing miasma theory continued to hinder progress, as efforts focused on mitigating “bad air” rather than targeting the actual vector (Bruce-Chwatt, 1988). This period represents a critical transition, where nascent scientific tools and observations began to chip away at long-held beliefs, setting the stage for the breakthroughs of the late 19th century.
The Parasite Revealed (1880–1900)
The true nature of malaria finally came to light with Alphonse Laveran’s landmark discovery in 1880. While stationed in Algeria, Laveran, a French Army surgeon, meticulously examined blood samples from malaria patients using a microscope. He observed parasitic organisms within the red blood cells, which he correctly identified as the causative agent of malaria. This discovery, detailed in his 1884 publication “Traité des fièvres palustres,” revolutionized malaria research, shifting the focus from environmental factors to a specific biological agent (Institute of Medicine (US) Committee on the Economics of Antimalarial Drugs, 2004; Laveran, 1881).
Building on Laveran’s work, the intricate relationship between malaria and mosquitoes began to unfold. Patrick Manson, whose work focused primarily on filariasis, proposed that mosquitoes might play a role in transmitting malaria. Inspired by Manson’s work, Ronald Ross, a British officer in the Indian Medical Service, embarked on a series of rigorous experiments in India. In 1897, he definitively demonstrated the transmission of avian malaria by mosquitoes, observing the development of the parasite within the Anopheles mosquito (Ross, 1910). This breakthrough earned him the Nobel Prize in Physiology or Medicine in 1902 and irrevocably linked mosquitoes to the spread of malaria. Shortly thereafter, Italian scientists, including Giovanni Battista Grassi, Amico Bignami, and Giuseppe Bastianelli, confirmed Ross’s findings in humans, demonstrating that Anopheles mosquitoes transmitted human malaria (Institute of Medicine (US) Committee on the Economics of Antimalarial Drugs, 2004). This period of rapid discovery laid the foundation for targeted interventions against malaria, focusing on mosquito control and disrupting the parasite’s life cycle.
The 20th Century: Control and Resistance (1900–2000)
The 20th century ushered in an era of unprecedented progress in malaria control, fueled by the newfound understanding of its transmission. Early efforts focused on interrupting the mosquito life cycle through environmental management, including drainage of swamps and larviciding. The discovery of quinine’s efficacy in the 17th century, though its mechanism of action remained unknown, provided the first effective treatment (Institute of Medicine (US) Committee on the Economics of Antimalarial Drugs, 2004). However, it was the development of synthetic antimalarials in the 20th century that truly revolutionized malaria treatment. The introduction of chloroquine in the 1930s offered a highly effective and readily available drug, followed by other synthetic antimalarials like mefloquine, primaquine, and pyrimethamine (Coatney, 1953).
Paul Hermann Müller’s discovery of DDT’s insecticidal properties in the 1940s provided a potent weapon against the mosquito vector. DDT spraying campaigns, coupled with drug treatments, formed the backbone of the Global Malaria Eradication Programme (GMEP) launched by the WHO in 1955. The GMEP successfully eliminated malaria from several regions and pioneered global health strategies, but its rigid, top-down approach that failed to adapt to diverse local conditions and insecticide resistance in mosquito populations, lead to resurgences and eventual abandonment of its eradication goal. Its legacy underscores the need for flexible, community-rooted, and research-integrated strategies in future elimination efforts (Müller, 1948; Nájera et al., 2011).
The latter half of the 20th century witnessed a resurgence of malaria in many areas, fueled by these challenges and compounded by factors like population growth, migration, and inadequate health infrastructure. The limitations of the GMEP highlighted the complexity of malaria control and the need for integrated, adaptable strategies. The emergence of drug resistance underscored the need for new antimalarials and emphasized the importance of understanding the parasite’s evolutionary dynamics. The experience of the 20th century laid the groundwork for the more nuanced and comprehensive approaches to malaria control that characterize the 21st century.
The Modern Era: New Challenges and Hope (2000-2025)
Malaria remains a global health challenge, particularly in sub-Saharan Africa. Drug resistance continues to emerge, requiring the development of new antimalarial combinations. The rollout of artemisinin-based combination therapies (ACTs) in the early 2000s provided a crucial tool, but resistance to artemisinin has already emerged. Insecticide-treated bed nets (ITNs) have become a cornerstone of malaria prevention. The development of the RTS,S malaria vaccine, approved by the WHO in 2021, represents a significant milestone, offering partial protection to young children (Dondorp et al., 2009; Lengeler, 2004; RTS,S Clinical Trials Partnership, 2015). Ongoing research focuses on new drugs, vaccines, and transmission-blocking strategies.
Conclusion: A Legacy of Perseverance
The fight against malaria has been a long and arduous journey, marked by both triumphs and setbacks. From ancient remedies to cutting-edge scientific research, humanity’s pursuit of understanding and combating this disease has driven remarkable progress. The journey continues, demanding continued investment in research, innovation, and global collaboration. As we move forward, a renewed commitment to malaria control and elimination remains essential to protect vulnerable populations and ultimately achieve a malaria-free world.
Please share your thoughts, interests and questions in the comments below or on the upper right side of the page.
Feel free to share this page on your preferred social media platforms using the sharing options conveniently located on this page.